Загрузил
aee
Topographic Anatomy & Operative Surgery Study Guide | Medical Lessons
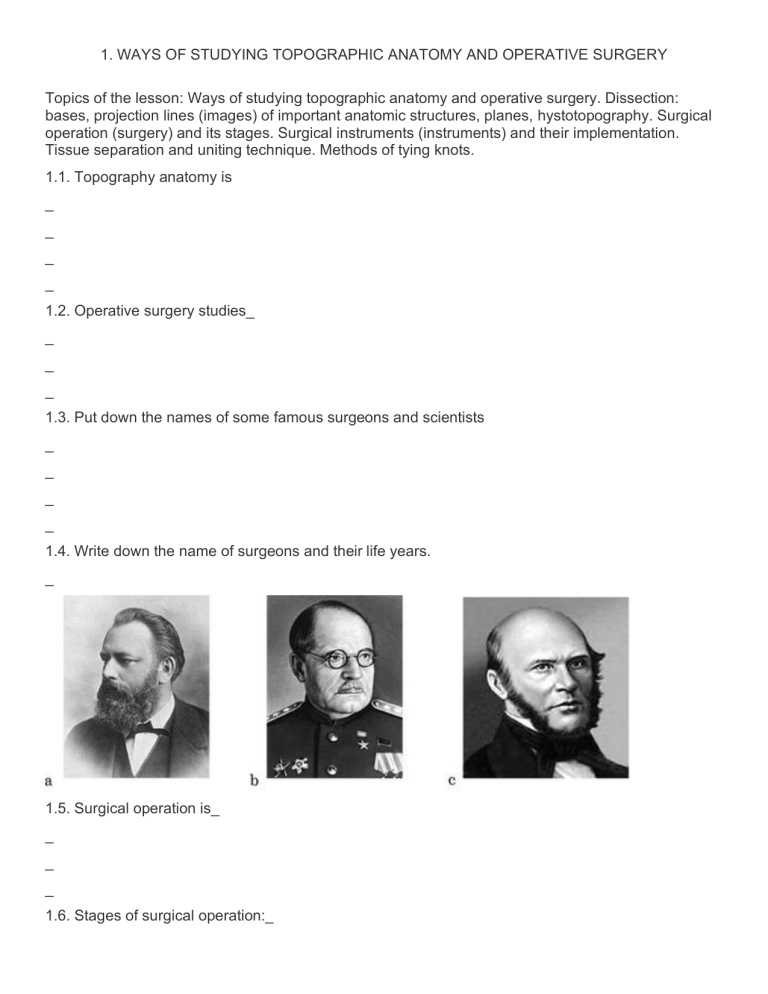
1. WAYS OF STUDYING TOPOGRAPHIC ANATOMY AND OPERATIVE SURGERY Topics of the lesson: Ways of studying topographic anatomy and operative surgery. Dissection: bases, projection lines (images) of important anatomic structures, planes, hystotopography. Surgical operation (surgery) and its stages. Surgical instruments (instruments) and their implementation. Tissue separation and uniting technique. Methods of tying knots. 1.1. Topography anatomy is _ _ _ _ 1.2. Operative surgery studies_ _ _ _ 1.3. Put down the names of some famous surgeons and scientists _ _ _ _ 1.4. Write down the name оf surgeons and their life years. _ 1.5. Surgical operation is_ _ _ _ 1.6. Stages of surgical operation:_ 1. __ 2. __ 3. __ 1.7. Put down: Incisio_ Tomia_ Stomia_ Sectio_ Punctio_ Ectomia_ Resectio_ Amputatio_ Exarticulatio_ Rrhaphia_ Trepanatio_ 1.8. Write down Holotopy_ Sintopy_ Sceletotopy_ 1.9. Classification of surgical equipment (name surgical equipment groups) _ _ _ _ _ _ _ _ _ _ 1.10. Put down the name of surgical instrument a)_ b)_ а -_ b -_ с -_ а)_ b)_ а)_ b)_ 1.11. Write down the positions of the scalpel 1. 2. 3. 1.12. Put down the right or wrong position of the needle in needle holder. a_ b_ c_ d_ 1.13. Choose the right position of the forceps. а_ 1.14. Write down the steps of skin incision. а_ _ b_ _ c_ _ 1.15. Put down the steps of fascia incision. b_ _ _ _ _ _ 1.16. Write down the steps to stop bleeding from wounds. 1_ 2_ 3_ 1.21. Name the type of sutures: 1_ 2_ 3_ 2. TOPOGRAPHIC ANATOMY AND OPERATIVE SURGERY OF SHOULDER GIRDLE: SUBCLAVIAN, AXILLARY, DELTOID, SCAPULAR REGIONS AND SHOULDER JOINT Topics of the lesson: Surface landmarks, borders of regions, general descriptions of regions. Scapular region: bone base, layers, supraspinous fossa and infraspinous fossa; fascial-cellular formations and their relationship with neighboring regions; blood supply and innervation. Deltoid region: layers; fascial-cellular formations; vessels, nerves, synovial bags. Subclavian region: layers, fascial-cellular formations, blood supply and innervation. Axillary region: borders; the walls of the axillary fossa; neurovascular formations; lymph nodes and ways of lymph outflow; triangular and quadrilateral foramen; connection of the axillary fossa with the cellular space of neighboring regions. Shoulder joint: articular capsule, its weak points, ligament apparatus; blood supply and innervation of the joint; position of the humeral head at dislocations; arterial collateral regions of the shoulder joint. 2.1. Draw the borders of scapular regions in Fig. 2.1 and name them: Superior_ _ _ Inferior_ _ _ Lateral_ _ _ Medial_ _ _ Fig. 2.1. Shoulder joint region 1 2.2. Using Fig. 2.2, name arteries, forming аscapular arterial ring and sign them on the Fig.: a) from the system of subclavian artery: 1__ _ 2__ _ b) from the system of axillary artery: 3__ _ 4__ _ Fig. 2.2. Arterial blood supply of scapular 2.3. How will collateral blood supply be carried out when there is a violation of blood flow through the axillary artery in case А, B and C (use Fig. 2.3)? А. __ _ _ B. __ _ _ C. __ _ _ Which two from these zones are preferable for ligation of axillary artery?_ _ _ _ _ _ _ Fig. 2.3. Ways of collateral blood supply at the axillary artery ligation 2.4. List the layers of scapular region, marked in Fig. 2.4, in English and Latin. Fig. 2.4. Topography of the scapular region 2.5. In Fig. 2.5, highlight in color the subclavian region and name its borders: Superior_ _ _ Inferior_ _ _ Medial_ _ _ Lateral_ _ _ Fig. 2.5. Regions of the upper limb 2.6. List the layers of subclavian region: 1. __ 2. __ 3. __ 4. __ 5. __ 6. __ 7. __ 8. __ 9. __ 10. __ 2.7. Name the structures in Fig. 2.6 in English and Latin. 2.8. Using Fig. 2.7, name the sides of triangles, in which the axillary artery goes. Fig. 2.6. Topography of the subclavian region Triangle А: name:_ borders:_ _ Triangle B: name:_ borders:_ _ Triangle C: name:_ borders:_ _ Fig. 2.7. Triangles of the subclavian and the axillary regions 2.9. Choose the correct answer: 1. Brachial plexus is formed from the roots С1-С4; 2. Brachial plexus is formed from the roots С5-Th1; 3. Brachial plexus is formed from the roots С1-Th1. 2.10. Name the structures in Fig. 2.8 in English and Latin. Fig. 2.8. Brachial plexus formation diagram 2.11. Explain the situation in this clinical case. In case of a clavicle fracture in the middle third with a displacement of fragments, it is necessary to perform transport immobilization - to bind the patient's elbows back. Give topographic and anatomical grounding of this method. How can a fracture of the clavicle in the middle third be complicated? _ _ Why and how will medial and lateral fragments be displaced (Fig. 2.9)? _ _ _ _ _ _ _ _ _ _ _ _ _ Fig. 2.9. Clavicle fracture with displacement 2.12. Highlight and name borders of the axillary region presented in Fig. 2.10: Anterior_ _ Dorsal_ _ Lateral_ _ Medial_ _ Fig. 2.10. Regions of the upper limb 2.13. Explain the situation in this clinical case. A patient with a knife wound in the axillary region was admitted to the surgical department. The wound 2 centimeters long is located in the transverse direction at the level of the inner margin of coracobrachialis muscle. Which nerve can be damaged? _ _ The function of which muscles and skin sensitivity of which regions need to be checked to clarify a diagnosis? _ _ _ _ _ 2.14. Name the structures that form the walls of the axillary fossa, using Fig. 2.11: А -_ _ B -_ _ Fig. 2.11. Walls of the axillary fossa C -_ _ D -_ _ What is the lower wall of the axillary fossa? _ _ 2.15. Write the names of the groups of lymph nodes in the axillary and subclavian regions in Fig. 2.12: 1 -_ 2 -_ 3 -_ 4 -_ 5 -_ 6 -_ Fig. 2.12. Groups of lymph nodes 2.16. Choose the correct answer. The lymph node, which serves as the first barrier of the lymph flow out from mammary gland and is affected by metastases at cancer is called: 1. Sorgius's node. 2. Pirogov's node. 3. Virchow's node. 2.17. Fill in the table «The spread of purulent discharge during inflammation of the subcutaneous adipose tissue of axillary region». AREA OF PURULENT EXUDATE SPREADING OUT FROM AXILLARY FOSSA: THE WAY OF SPREADING DOWN THE ANATOMICAL STRUCTURES: 1. In subdeltoid region 2. In subscapular region 3. In subclavian region, under the pectoralis major muscle to the anterior pectoral wall 4. In lateral cervical region 5. Into anterior fascial muscular bed of the shoulder 6. Into posterior fascial muscular bed of the shoulder 2.18. Explain the situation that happened in this clinical case. A 35-years-old patient was admitted to the traumа department with a dislocated shoulder in the shoulder joint. After the dislocation was repositioned, the patient could not take the shoulder to the horizontal level, but the passive abduction remains. Also, the skin sensitivity of the deltoid region is not detected. Give a topographic and anatomical grounding for the arising symptoms. _ _ _ _ _ 2.19. Using Fig. 2.13, fill in the table. Fig. 2.13. Puncture points of the shoulder joint 1. Indications: Puncturing of the shoulder joint Diagnosis – _ _ _ Treatment – _ _ _ 2. Limb position: 3. Type of anesthesia: 4. Points of needle injection: a) Anteriorly – b) Laterally – c) Posteriorly - Direction of needle: 3. TOPOGRAPHIC ANATOMY AND OPERATIVE SURGERY OF ANTERIOR AND POSTERIOR REGIONS OF THE SHOULDER, ELBOW AND FOREARM Topics of the lesson: Shoulder region: borders, layers, fascial-cellular formations; topography of the neurovascular structures of the shoulder; position of fragments at humerus fractures. Elbow region: borders, layers, cubital fossa; fascial formations. Elbow joint: articular capsule, its weak points, ligament apparatus; blood supply and innervation of the elbow joint; position of the bones at joint dislocation. Forearm region: borders, layers, fascial-cellular formations; topography of the neurovascular structures; position of fragments at forearm bones fractures. Distal radioulnar joint: borders, articular capsule, its weak points, ligament apparatus; synovial sheaths of tendon; blood supply and innervation of the joint. 3.1. Highlight in different colors and draw the borders of anterior and posterior regions of the shoulder in Fig. 3.1: Fig. 3.1. Regions of the upper limb Superior_ Inferior_ Lateral_ Medial_ 3.2. Determine which third of the shoulder (upper, middle, or lower) is featured in Fig. 3.2 and name structures in English and Latin. Fig. 3.2. Topography of the shoulder region 3.3. Sign the names of the nerves that provide cutaneous innervation of the V-X zone in Fig. 3.3. Fig. 3.3. Zones of cutaneous sensitivity of the upper limb № Name in english Name in latin V VI VII VIII IX X 3.4. Explain the situation in this clinical case. During training, the gymnast was injured: displacement of the humeral head. What direction of displacement of the humeral head is most likely and why? Give a topographic and anatomical justification. _ _ _ _ _ _ 3.5. Choose the correct answer. The content of the posterior fascial compartment of the arm is: 1) biceps brachii muscle; 2) triceps brachii muscle; 3) coracobrachialis muscle; 4) pronator teres muscle; 5) brachialis muscle. 3.6. Based on the topography of the brachial artery draw: a) an artery projection line; b) indirect access to it in Fig. 3.4. What vein can be damaged at the projection access to the brachial artery? _ _ Fig. 3.4. Lateral elevated upper limb 3.7. Using Fig. 3.5, name vessels involved in the blood supply of the elbow joint. Fig. 3.5. Artery blood supply of the elbow joint 3.8. Using Fig. 3.6, fill in the table. Fig. 3.6. Puncture points of the elbow joint Puncturing of the elbow joint 1. Indications: - 2. Limb position: 3. Type of anesthesia: 4. Points of needle injection: Direction of needle: A) Posteriorly – B) Laterally – 3.9. Explain the situation happened in this clinical case. The correct choice of site for intravenous injection is the anterior ulnar region (Fig. 3.7). Fig. 3.7. Intravenous injection in the elbow region Which vein is punctured during the injection? Give a topographic anatomical grounding for the choice of this vein for manipulation. Why is the puncture of basilic vein and cephalic vein dangerous? _ _ _ _ _ _ _ _ _ _ 3.10. In Fig. 3.8, draw the projection lines of the radial and ulnar arteries. Fig. 3.8. Lateral elevated upper limb 3.11. Fill in the table using Fig. 3.9. Name the muscles of the anterior and posterior regions of the forearm, their function, indicate the nerve involved in the innervation of these muscles, name the main vessels and nerves of the forearm. Fig. 3.9. The topography of anterior and posterior forearm regions № muscle name function innervation Anterior region of forearm, 1st layer 1 2 3 * Anterior region of forearm, 2nd layer 4 Anterior region of forearm, 3rd layer 5 6 Anterior region of forearm, 4th layer * Posterior region of the forearm, the surface layer 7 8 9 10 11 Posterior region of the forearm, deep layer 12 13 14 Lateral fascial compartment 15 * name in english name in latin Arteries and nerves of the anterior fascial compartment А1 N1 A2 N2 A3 N3 A4 N4 Arteries and nerves of the posterior fascial compartment A5 N5 Bones and fascial structures U R 16 * - muscles of the forearm that are not shown in a given cross-section. 3.12. Explain the situation in this clinical case. The soft tissues of the lower third of the anterior region of the forearm are damaged by a sharp fragment of a glass. A deep wound is located in the middle of the distance between the styloid processes of radial and ulnar bones and has a transverse direction. What structure can be damaged? The function of what nerve and what muscles should be checked to specify the diagnosis (given that the nerve is damaged in the lower third)? _ _ _ _ _ _ _ _ _ _ 3.13. Fill in the table. Nerve name Damage symptoms (clinical picture) Topographic and anatomical grounding Radial nerve Ulnar nerve Median nerve Musculo-cutaneous nerve 3.14. Describe where the cellular space of Pirogoff-Parona is located and how the infection spreads when it becomes inflamed. Region:_ Walls:_ _ _ Ways of spreading pus:_ _ _ 3.15. Using Fig. 3.10, name what forms: a) carpal tunnel_ _ b) Guyon's canal_ _ Fig. 3.10. Canals of the wrist 3.16. Fill in the table. osteofibrous tunnels of the anterior region of the wrist canal name 1 Carpal tunnel 2 Guyon's canal content The contents of osteofibrous tunnels of the posterior region of the wrist № № 1 2 3 4 5 6 3.17. Explain the situation in this clinical case. Patient N., 38 years old, slipped and fell on his wrist. After that she was taken to the intensive care unit, where the woman underwent X-ray examination (Fig. 3.11). Based on the anatomical structure of the radial and ulnar bones, diagnose which bone is fractured and in which part? _ _ _ Fig. 3.11. X-ray examination of the left hand in anterior and lateral projections 4. TOPOGRAPHIC ANATOMY AND OPERATIVE SURGERY OF THE REGION OF THE HAND Topics of the lesson: The region of the hand: topography of the palm and dorsum of the hand; fascialcellular formations and their relationship with neighboring regions; blood supply and innervation of the region; projection of the arterial arches; synovial and bone-fibrous sheaths of finger flexor tendons. Purulent processes of hand and digits: classification; local anesthetic methods; cuts for drainage. 4.1. Highlight the palm region in Fig. 4.1, name the borders. Superior_ _ Inferior_ _ Fig. 4.1. External landmarks of the palm region 4.2. Draw on the Fig. 4.1 the projections of superficial and deep palmar arterial arches, median nerve and the forbidden zone of Kanavel. 4.3. List the layers of the palm region of the hand: 1. Skin -_ 2__ 3. _ 4. _ 5. _ 6. _ 7. _ 8. _ 9. _ 10. _ 11. _ 12. _ 4.4. Using Fig. 4.2, name the arteries forming superficial and deep arterial arches and sign them in the Fig.: Fig. 4.2. Arterial blood supply of the palm 4.5. Fill in the table using Fig. 4.3. Name what forms the fascial compartment of the hand that passes through them. Fig. 4.3. The transverse section of the wrist NAME WALLS CONTENT Middle compartment of palm Anterior – Tendons: Posterior – Arteries: Medial – Nerves: Lateral - Muscles: Anterior – Tendons: Lateral compartment of palm Posterior – Muscles: Medial - Lateral - Medial compartment of palm Anterior – Posterior – Medial - Lateral - Muscles: 4.6. Using Fig. 4.4, fill in the table. Fig. 4.4. Puncture of the wrist joint puncture of the wrist joint 1. Indications: - 2. Limb position: 3. Type of anesthesia: puncture of the wrist joint 4. The point of puncture: Direction of needle: The intersection points of the lines: А-B- External reference points: а) bones: 1. 2. b) tendons: 3. 4. 4.7. Explain the situation in this clinical case. As a result of the corn abscess of the 2nd interdigital space, the pus has spread into the palm commissural opening. In what layer is the abscess located now? _ _ Specify the ways of further spread of purulent leak (distal, proximal). _ _ _ _ 4.8. In Fig. 4.5, draw lines to indicate incisions in the subcutaneous felon (panaritium) of the middle and distal phalanges and in the commissural phlegmon. Fig. 4.5. Incisions in the subcutaneous felon Fig. 4.6. Incisions according to Klapp 4.9. What is tendovaginitis?_ _ _ _ 4.10. In Fig. 4.6, draw projections of the synovial sheaths of the II-IV fingers and incisions for drainage of the tendovaginitis according to Klapp. 4.11. What are the radial and ulnar tendobursites? _ _ _ 4.12. In Fig. 4.7, draw the projection of the radial and ulnar synovial bursae and incisions for ulnar and radial tendobursites. 4.13. In Fig. 4.8, mark with a pencil the lines of incisions for opening of the subaponeurotic phlegmon of the middle compartment according to Voyno-Yasenetsky-Pick. Consider the forbidden zone! Fig. 4.7. Incisions for radial and ulnar synovial bursae Fig. 4.8. Incisions according to Voyno-Yasenetsky-Pick 4.14. Indicate in Fig. 4.9 point of the needle puncture during the blockade according to OberstLukashevich and Usoltseva. What nerves are blocked in this case? _ _ _ _ _ _ Fig. 4.9. Dorsum surface of the hand 4.15. Blockades of which nerves are shown in Fig. 4.10. Describe the points for the blockade. a)_ _ b)_ _ Fig. 4.10. Conductive anesthesia of the wrist c)_ _ 4.16. In Fig. 4.11, mark with pencil incisions with the periungual paronihia and different variants of subungual panaritium. Paronihia is_ Panaritium is_ Fig. 4.11. Distal phalange 4.17. What tendons are marked with the letters «A» and «B» in Fig. 4.12? What is the name of the zone marked with the letter «C»? What anatomical formations are projected onto it? А -_ B -_ C -_ Fig. 4.12. Lateral surface of the hand - «anatomical snuffbox» 4.18. List the layers of the dorsum surface of the hand using Fig. 4.13: Fig. 4.13. The transverse section of the hand 4.19. List the layers and structure of fingers using the Fig. 4.14. What type of subcutaneous cellular space is located on the palmar surface of the fingers? _ _ What is the clinical significance?_ _ Fig. 4.14. Layered structure of the finger 5. TOPOGRAPHIC ANATOMY AND OPERATIVE SURGERY OF THE FRONT AND BACK OF THE THIGH, GLUTEAL REGION AND HIP JOINT Topics of the lesson: Topographic anatomy and operative surgery of the front and back of the thigh, gluteal region and hip joint. Accesses to the neurovascular bundle of the lower limb. Puncture of the hip joint. 5.1. Highlight and name the borders of anterior and posterior regions of thigh in the Fig. 5.1: Superiorly_ _ Inferiorly_ _ Laterally_ _ Medially_ _ Fig. 5.1. The regions of lower limb 5.2. Shade femoral triangle (Scarpa's Triangle) and name its borders on the Fig. 5.2. Superiorly_ _ Medially_ _ Laterally_ _ Fig. 5.2. The topography of the femoral triangle 5.3. Name the structures according to the Fig. 5.3 in English and Latin. Fig. 5.3. Surface structures of the femoral triangle 5.4. Highlight the fascial compartments of thigh shown in Fig. 5.4 and name the muscles located there. № Name of the muscle Function Anterior - the extensor compartment of thigh Medial - the adductor compartment of thigh Posterior - the flexor compartment of thigh Fig. 5.4. Fascial compartments of thigh in a transverse section in the upper third 5.5. Using Fig. 5.5, describe the topography of the muscular and vascular spaces. Fig. 5.5. The muscular and vascular spaces of the thigh Muscular space (lacuna musculorum) Anteriorly: Posteriorly: Medially: Content: Vascular space (lacuna vasorum) Anteriorly: Laterally: Medially: Posteriorly: Content: - 5.6. In Fig. 5.6, mark the projection line of the femoral artery (Ken line), and mark with color the femoral artery and its branches. Fig. 5.6. Bones of the lower limb 5.7. Using Fig. 5.7, describe the topography of the femoral canal. Fig. 5.7. Femoral canal and a femoral hernia THE WALLS OF THE FEMORAL CANAL Anterior Posterior Lateral BORDERS OF THE DEEP FEMORAL RING Anterior Posterior Medial Lateral SUPERFICIAL FEMORAL RING IS FORMED BY - 5.8. Using Fig. 5.8, describe the topography of the adductor canal (Hunter). ADDUCTOR CANAL WALLS: FORMED BY: 1 2 3 OPENING OF THE CANAL FORMED BY STRUCTURES INSIDE 1 2 3 Fig. 5.8. Explain the situation in this clinical case 5.9. Explain the situation in this clinical case. The patient was diagnosed with cellulitis of the anterior fascial compartment of thigh. Specify the possible ways of dissemination of purulent discharge. Upper_ _ Lower_ _ Laterally_ _ Medially_ _ Posteriorly_ _ In the subcutaneous_ _ 5.10. Using Figs. 5.9 and 5.10 name the borders and layers of the gluteal region. Fig. 5.9. Topography of the gluteal region THE BORDERS OF THE GLUTEAL REGION: Superior Inferior Lateral Medial Fig. 5.10. Topography of the gluteal region LAYERS OF THE GLUTEAL REGION: THE NAME OF MUSCLE А. Superficial muscle layer 1 B. Middle muscle layer 1 2 3 4 5 6 C. Deep muscle layer 1 2 BLOOD SUPPLY AND INNERVATION OF THE MUSCLE 5.11. In Fig. 5.11, draw the projection lines of the suprapiriform and infrapiriform foramens. Fig. 5.11. Projection of the neurovascular bundles on the skin of the gluteal region 5.12. List the neurovascular bundles extending from the suprapiriform and infrapiriform foramens, starting from the lateral side, according to their relative positions. Use Fig. 5.11. A. From suprapiriform opening:_ B. From infrapiriform opening: 1. __ 2. __ 3. __ 4. __ 5.13. Explain the situation happened in this clinical case. In a patient with post-injection abscess of the gluteus, the pus has spread into the ischiorectal fossa. Give anatomical grounding. _ _ _ _ _ 5.14. List the hip joint ligaments using Fig. 5.12. Рис. 5.12. Ligaments of the hip joint: A - intra-articular, B - extra-articular THE NAME OF THE LIGAMENT IN ENGLISH THE NAME OF THE LIGAMENT IN LATIN Intra-articular Extra-articular ligaments 5.15. Explain the situation in this clinical case. The patient complains about the pain in the lower limb that occurs after passing 50 m (the «intermittent claudication» symptom). During the examination, the pulsation on the femoral artery under the inguinal fold is distinct, on the popliteal artery and on the arteries of the foot it is not determined. Angiography obtained an image of the femoral artery up to the level of the middle third of the thigh. The popliteal artery is filled up through the well-defined collateral ways. What arteries provide the blood supply for the extremity below the level of the obliteration? Use Fig. 5.13. _ _ _ _ _ _ _ _ _ _ Рис. 5.13. Collateral ways of the hip joint 5.16. Using Fig. 5.14, fill in the table. Puncture of the hip joint 1. Indications: 2. Limb position: 3. Type of anesthesia: 4. Puncture points of the hip joint: А) Outside B) In front - Needle direction: Рис. 5.14. Puncture points of the hip joint 5.17. Explain the situation in this clinical case. During surgery for a strangulated femoral hernia, profuse bleeding occurred. The defect in the vessel wall was sutured. In the postoperative period, there was swelling of the entire lower limb. What mistake was made by the surgeon? What is the cause of swelling? _ _ _ _ _ _ _ _ _ _ 5.18. In Fig. 5.15, draw the projection line of the sciatic nerve. Mark a point for the blockade of this nerve. Рис. 5.15. Posterior thigh region 6. TOPOGRAPHIC ANATOMY AND OPERATIVE SURGERY OF ANTERIOR AND POSTERIOR REGIONS OF KNEE, KNEE JOINT AND LEG Topics of the lesson: Topographic anatomy of anterior et posterior regions of knee, knee joint and leg. Approaches to the main neurovascular bundles of regions. Puncture of knee joint. 6.1. Highlight and name the borders of the anterior et posterior regions of the knee, represented in the Fig. 6.1: Superior_ _ Inferior_ _ Lateral_ _ Medial_ _ Fig. 6.1. Regions of the lower limb 6.2. Using the Fig. 6.2, name the borders of the popliteal fossa and name the elements of the neurovascular bundle. Borders: Superolateral_ _ _ Inferomedial_ _ _ Fig. 6.2. Topography of the popliteal fossa Inferolateral_ Inferolateral_ _ _ Superomedial_ _ _ 6.3. Explain the situation happened in this clinical case. Atherosclerosis led to occlusion of the popliteal artery above the place of origin of the upper articular branches. Explain how the blood supply of leg and foot can be preserved. Use the Fig. 6.3. _ _ _ _ _ _ _ _ _ _ Fig. 6.3. Blood supply of the knee joint 6.4. List the ligaments of the knee joint, using the Fig. 6.4. Fig. 6.4. Ligaments of the knee joint Name of the ligament in english Name of the ligament in latin Intra-articular Extra-articular 6.5. List the recesses of the knee joint. Anterior recesses: Posterior recesses: Lateral recesses: Lateral recesses: 6.6. Highlight the fascial compartments of leg, represented in the Fig. 6.5, and name the muscles located in them. fascial compartments of the leg in the transverse section № Name of the muscle Function Anterior fascial compartment of the leg Lateral fascial compartment of the leg Posterior fascial compartment of the leg Innervation Fig. 6.5. Fascial compartments of the leg in the transverse section 6.7. Explain the situation in this clinical case. The patient came to the surgeon with complaints of impaired sensitivity along the external surface of the lower third part of leg and the dorsal side of the foot. On the border between the middle and lower third parts of the leg external surface there is a rough scar of the former injury. The scar is located horizontally, the length of scar is 5 cm. Can the patient?s complaints be connected with the former wound? What structure could be injured, in what layer is it located? Use the Fig. 6.6. _ _ _ _ _ _ _ _ _ _ _ Fig. 6.6. Cutaneous sensitivity zones of the lower limb 6.8. Using the Fig. 6.7, note the superficial veins of the leg. Fig. 6.7. Superficial veins of the leg 6.9. Fill in the table. Describe the leg canals topography (Fig. 6.8). NAME OF THE CANAL 1. 2. 3. 4. WALLS CONTENTS Fig. 6.8. Canals of the leg 6.10. Fill in the table. NAME OF THE NERVE SYMPTOMS OF INJURIES (CLINICAL PICTURE) TOPOGRAPHICANATOMICAL GROUNDING Tibial nerve Common fibular nerve Deep fibular nerve Superficial fibular nerve Fig. 6.9. Symptoms of nerves injuries Fig. 6.10. Puncture of the knee joint 6.11. Fill in the table PUNCTURE OF THE KNEE JOINT 1. Indications 2. Limb position 3. Type of the anesthesia 4. Incision point: А) Superolateral - B) Superomedial - C) Inferolateral - D) Inferomedial - Direction of the needle: 6.12. Describe the sequence of surgeon actions during the venectomy. Describe the methods of ligating perforating veins. _ _ _ _ _ _ _ _ _ _ 6.13. Explain the situation in this clinical case. During the examination of a patient in a hospital, the traumatologist found out, that the superior proximal part of the leg can move forward relative to the thigh. Give the topographic-anatomical grounding. What if the proximal part of the leg moves backward in relation to the thigh? _ _ _ _ _ _ _ _ _ _ 7. TOPOGRAPHIC ANATOMY AND OPERATIVE SURGERY OF THE ANKLE JOINT, LATERAL AND MEDIAL RETROMALLEOLAR REGIONS, FOOT Topics of the lesson: Topographic anatomy of the anteromedial and posterior areas of the ankle joint. Access to the main neurovascular bundles of the areas. Puncture of the ankle joint. 7.1. In Fig. 7.1, mark with color and indicate the borders of the ankle joint region. Fig. 7.1. Ankle joint region Upper_ _ Lower_ _ 7.2. In Fig. 7.2, mark the projection line of the dorsal pedis artery and deep peroneal nerve. Fig. 7.2. Front view of the foot 7.3. Indicate the anteroposter structures located in the medial malleolar canal and indicate them with numbers using Fig. 7.3. Fig. 7.3. The medial retromalleolar region а_ b_ c_ d_ 7.4. Explain the situation in this clinical case. Atherosclerosis led to occlusion of the popliteal artery above the origin of the upper articular branches. Explain how the blood supply of leg and foot can be maintained. Use Fig. 7.4. Specify the arteries indicated with numbers. _ _ _ _ _ _ _ 1_ 3_ 4_ 6_ Fig. 7.4. Back view of the leg 7_ 18_ 20_ 21_ 7.5. In Fig. 7.5, specify the projection line of the posterior tibial artery. In what position of the foot will it be better to palpate this artery and in the case of which complaints of the patient? _ _ _ 7.6. Specify the nerves innervating the dorsum of foot according to the numbers in Fig. 7.6. 1. _ _ 2. _ _ 3. _ _ 4. _ _ 5. _ _ Fig. 7.5. The medial retromalleolar region innervation of the dorsum of foot Fig. 7.6. The skin 7.7. Explain the situation happened in this clinical case. The patient came to the surgeon with the complaints of sensitivity disorders along the external surface of the lower third part of leg and the dorsal side of the foot. On the border between the middle and lower third parts of the leg external surface there is a rough scar of the former injury. The scar is located horizontally, the length of scar is 5 cm. Can the patient?s complaints be connected with the former wound? What structure could be injured, in what layer is it located? _ _ _ _ _ _ _ _ 7.8. Using Fig. 7.7, select the footprint typical for the flat feet. 7.9. In Fig. 7.8, make the projection lines of the lateral and medial plantar tracts. Fig. 7.7. Images of the footprints Fig. 7.8. Foot images 7.10. Specify the nerves innervating of the foot skin using Fig. 7.9. 14. __ 15. __ 16. __ 17. __ 7.11. Specify the structures shown on the foot cross-section at the level of the tarsus in English and Latin. Fig. 7.9. Innervation of the foot skin Fig. 7.10. The transverse section of foot at the level of the tarsus 7.12. Explain the situation in this clinical case. During the football match, the football player got injured - fracture of the neck of the fibula. During examination, the foot is in the plantar flexion position, its external margin is lowered. What nerve is damaged? Describe the place of injury and symptoms, give the topographic and anatomical grounding. _ _ _ _ _ _ _ _ 8. AMPUTATION SURGERY ON LIMBS. WAYS OF SOFT TISSUES TREATING DURING AMPUTATIONS, TENORRHAPHY Topics of the lesson: The concept of amputations, exarticulations. Classification of amputations. The main stages of amputations and exarticulations. Types of treating of vessels, nerves, periosteum, bone, myorrhaphy, tenorrhaphy, stump formation. 8.1. Give definitions. Amputation is_ _ _ Exarticulation is_ _ _ 8.2. Using the Fig. 8.1, name the possible soft tissues dissection methods. Fig. 8.1. Soft tissue dissection during amputation 1. __ 2. __ 3. __ 4. __ 5. __ 8.3. The thigh circumference is 24 cm. Calculate the circumference of the long flap during the amputation of the thigh in the upper third. _ _ _ _ 8.4. Fill in the table. GRITTI-SZYMANOWSKI-ALBERCHT OSTEOPLASTIC THIGH AMPUTATION Definition:_ _ _ _ _ _ _ Indications: Special surgical set of instruments: 1. _ _ 2. _ _ 3. _ _ 4. _ _ 5. _ _ 1. Stage - Describe the flap formation technique _ _ _ _ _ _ _ 2. Stage _ Describe the technique of bone sawing, periosteum and patella treatment _ _ _ _ _ _ 3. Stage _ Describe the neurovascular tracts treating technique _ _ _ _ _ _ Fasciae and muscles suturing _ _ Skin suturing _ Limb immobilization PIROGOV?S OSTEOPLASTIC FOOT AMPUTATION Definition:_ _ _ _ _ _ _ Indications: Special surgical set of instruments: 1. _ _ 2. _ _ 3. _ _ 4. _ _ 5. _ _ 1. Stage Describe the flap formation technique 2. Stage Describe the technique of the leg bones sawing, periosteum treating and mapping of the heel bone 3. Stage Describe the technique of the treating of anterior and posterior neurovascular tracts Fasciae and muscles suturing _ Skin suturing _ Limb immobilization GÜnther osteoplastic amputation Is -_ Definition: _ _ _ _ _ Features that distinguish this amputation from the Pirogov?s foot amputation _ 1. 2. Sharpe foot amputation 1. Indications: 2. Cut out a skin flap from the remaining areas; 3. Treat the periosteum; 4. Saw the metatarsal bones at the base; 5. Cut out the plantar skin flap; 6. Treat the vessels and nerves on the rear and on the sole of the foot; 7. Cover the sawdust of the bones with a plantar flap isolation of the foot in the tarsometatarsal (lisfranc’s) joint 1. Cut the rear skin flap out and pull it off proximally; 2. Bend the foot as far as possible towards the sole and medially, open from the 5th to the 3rd tarsometatarsal joints; 3. Open the I tarsometatarsal joint; 4. Cut the ligaments of the II metatarsal bone, open the Lisfranc?s joint fully; 5. Cut the plantar skin flap out; 6. Cut down the protruding area of the I sphenoid bone; 7. Treat the vessels, nerves of the rear and the sole of the foot; 8. Connect plantar and dorsal skin flaps 8.5. Describe the general principles of tendon suturing and the author's technique of tendon suturing, represented in the Fig. 8.2. Fig. 8.2. Types of tendon sutures General principles:_ _ _ _ _ _ _ Types of tendon sutures: 1. _ 2. _ 3. _ 4. _ 5. _ 9. TOPOGRAPHIC ANATOMY AND OPERATIVE SURGERY OF CEREBRAL REGION OF THE HEAD Topics of the lesson: Cerebral cranium. Division into parts: cranial vault (calvaria, cranial fornix, skullcap or dome) and cranial base. Frontal-parietal-occipital region, temporal region: its borders, layers, blood vessels, nerves, lymphatic drainage. Blood supply to the soft tissues of the cranial vault. Cellular spaces (a.k.a subfascial cellular tissue) and their connections with cellular spaces of neighboring areas. Bone structure of the cranial vault. Diploicveins. Mastoid region: borders, layers, blood vessels, nerves. Triangle of Chipault. Facial nerve pathways. Meninges of the brain: dura mater, arachnoid mater, pia mater. Intermeningeal spaces: epidural, subdural, subarachnoid. Dura mater: its sinuses and connection with extracranial veins. Middle meningeal artery. Projection of structures on skull?s interior surface: arteria meningea media, dura mater sinuses, main sulci and gyri of cerebral hemispheres, brain?s ventricules (using Kronlein-Brusov?s scheme). Blood supply of the brain: Circle of Willis. Cerebral spinal fluid production and lymphatic drainage. Trepanation of the skull (a.k.a. making a burr hole). Trepanation of the mastoid process. Management of hemostasis in patients with head injuries. 9.1. Using Fig. 9.1, name the head regions and shade them in with different colors. Which region is not highlighted in this picture? Fig. 9.1. Regions of the head 9.2. In Fig. 9.2 highlight in color the frontal-parietal-occipital region and name its borders. Show projections of main arteries in this region and sign them on the picture. Fig. 9.2. Regions of the head Frontal_ _ _ Lateral_ _ _ Posterior_ _ _ 9.3. Using the Fig. 9.3, list anatomical structures on English and Latin languages. Fig. 9.3. Coronal section of the head though upper sagittal sinus 9.4. In Fig. 9.4, highlight in color the temporal region and name its borders. Show and name the projections of main artery and nerve. Fig. 9.4. Regions of the head Frontal_ _ _ Superior_ _ _ Posterior_ _ _ Inferior_ _ _ Artery and nerve_ _ _ 9.5. List the anatomic structures shown in Fig.9.5. Fig. 9.5. Layered structure of temporal region (scheme) 9.6. Fill in the table. cellular spaces of temporal region name connection with adjacent spaces 1 - 2 - 3 - 9.7. On the Fig. 9.6, draw the projection of the mastoid process's quadrants and write down which anatomic structures project in them. Fig. 9.6. Mastoid region of the head № QUADRANT ANATOMIC STRUCTURES 1 2 3 4 9.8. In the Fig. 9.7, show the Triangle of Chipault (a.k.a. trepanation triangle), describe its borders and clinical relevance. Fig. 9.7. Mastoid region of the head 1. Superior limit:_ _ 2. Anterior limit:_ _ 3. Posterior limit:_ _ Clinical relevance for triangle of Chipault:_ _ 9.9. Using Fig. 9.8, highlight the arteries that form circle of Willis. Name the arteries supplying the flood flow to the brain. Рис. 9.8. Circle of Willis 9.10. Name sinuses and their connected veins presented on the Fig. 9.9. 9.11. What other venous sinuses are not represented in Fig. 9.9 do you know? _ _ _ Fig. 9.9. Sinuses of dura mater 9.12. Using the Fig. 9.10, describe the lines necessary to make Kronlein-Brusov?s scheme. A. Horizontally: 1. __ 2. __ B. Sagittally: 3__ Fig. 9.10. Kronlein-Brusov?s diagram C. Vertically: 4. __ 5. __ 6. __ D. Diagonally: 7. __ 8. __ 9. __ 9.13. On the Fig. 9.10, draw and name the projections of blood vessels and important anatomical structures of brain that can be seen on Kronlein-Brusov?s diagram. _ _ _ _ 9.14. Name the locations of soft tissue hematomas of cranial vault, presented on the Fig. 9.11. Fig. 9.11. Hematomas 1. This hematoma is located in:_ _ 2. This hematoma is located in:_ _ What other types of hematomas are possible in cranial vault? _ _ 9.15. Use these pictures to describe how to stop bleeding in case to damage of dura mater`s sinuses. A. _ _ _ _ B. _ _ _ _ C. _ _ _ _ 9.16. Give the definition. Trepanation (trepanning, making a burr hole) is: _ _ _ 9.17. Fill in the table. 1. CRANIAL TREPANATION TYPE OF TREPANATION CLINICAL INDICATION - 2. - 9.18. Name surgical instruments used for trepanation presented in Fig. 9.12. SPECIAL SURGICAL INSTRUMENTS FOR CRANIAL TREPANATION FOR OSTEOPLASTIC CRANIAL TREPANATION FOR RESECTION (DECOMPRESSION) CRANIAL TREPANATION № № 1 1 2 4 3 5 6 Fig. 9.12. Special surgical instruments 9.19. Describe main steps of osteoplastic trepanation by Olivecrona. Step I _ _ _ _ _ Step II _ _ _ _ _ Step III _ _ _ _ _ Step IV _ _ _ _ _ 9.20. Describe the main steps of decompressive trepanation by Cushing. Step I _ _ _ _ _ Step II _ _ _ _ _ Step III _ _ _ _ _ Step IV _ _ _ _ _ 10. TOPOGRAPHIC ANATOMY AND OPERATIVE SURGERY OF THE FACIAL REGIONS OF THE HEAD Topics of the lesson: Facial regions. Face innervation. Projections of the branches of the trigeminal and facial nerve. Blood supply and venous outflow. Projections of facial vessels. Venous anastomoses. Lymph nodes. Muscles and fascia of the face. Topography of the parotid gland. The Bichat's fat pad of the cheek. Deep face area. Cellular spaces of the face. The spread of purulent processes. Complications of purulent parotiditis. Incision and drainage phlegmon. Primary surgical treatment of facial wounds. 10.1. Using Fig. 10.1, define face regions in English and Latin languages. Shade them in different colors. Fig. 10.1. Face regions 1. __ 2. __ 3. __ 4. __ 5. __ 6. __ 7. __ 8. __ 10.2. Highlight buccal region and define its borders. Draw projections of the main arteries of this area and mark them in the picture. Fig. 10.2. Face regions Frontal_ Superior_ Posterior_ Lower_ 10.3. Using Fig. 10.3, sign anatomic structures according to the numbers in English and Latin languages. Рис. 10.3. Facial bones 10.4. Highlight the parotid-masseteric region (regio parotideomasseterica) and define its borders. Draw projections of the main nerves of this area and mark them in the picture. Frontal_ _ Posterior_ _ Inferior_ _ Superior_ _ Fig. 10.4. Facial regions 10.5. Which cranial nerve innervates muscles used for facial expression (facial muscles)? _ Which cranial nerve innervates muscles of mastication? _ What nerve branches provide sensory innervation? _ 10.6. Mark the terminal (cutaneous) branches of the trigeminal nerve in the Fig. 10.5. 1. _ _ 2. _ _ 3. _ _ 4. _ _ Fig. 10.5. The trigeminal nerve branches 10.7. Using Fig. 10.6, name the arteries. What large artery do these branches make up? Fig. 10.6. Arteries of the head 10.8. Using Fig. 10.7, describe venous anastomoses in the nasolabial triangle («danger triangle» or «death triangle») Fig. 10.7. Venous anastomoses of the head Facial venous anastomoses pathways: Pathway а Pathway b Pathway с 1) Facial vein 1) Facial vein 1) Facial vein 2)_ 2)_ vein .3) _ vein vein 3)_ 2) _ vein 4) _ venosus sinus 4)_ 4) _ vein 5)_ 5)_ venosus sinus vein 6) _ venosus sinus venosus plexus 3)_ venosus plexus Why is an inflammation in this area considered to be dangerous? What life-threatening complications can it cause?_ _ _ _ Why are retrograde flow of blood and thromboembolism possible on the face? _ _ 10.9. Using Fig. 10.8, list the facial nerve branches. Where is the projection point of facial nerve exit to the face? The branches of a facial nerve are: 1. _ 2. _ 3. _ 4. _ 5. _ 6. _ 7. _ 8. _ 9. _ Fig. 10.8. Facial nerve branches 10.10. Using Fig. 10.9, describe the localization of buccal fat pad (Bichat's fat pad) and its temporal process (a). What other processes does this buccal fat pad have? b)_ c)_ Fig. 10.9. Buccal fat pad (Bichat's fat pad) 10.11. Using Fig. 10.10, list the nerves that control innervation of the upper jaw, lower jaws and teeth. Fig. 10.10. Teeth innervation 10.12. Using Fig. 10.11, draw the parotid gland duct. What is another name for this duct?_ _ What muscle does it pass through?_ _ Where does its duct open?_ _ Fig. 10.11. Parotid gland duct 10.13. List the anatomical structures that are located in the middle of the parotid salivary gland. Fill in the table; write the symptoms and complications caused by compression of these structures during purulent parotitis. Parotid salivary gland topography Anatomical structure Symptoms and complications Arteries: _ _ _ Veins: _ _ _ Nerves: _ _ _ Lymph nodes: _ _ _ 10.14. What are the weak points in the capsule of parotid gland? Where the purulent process can spread through these points. weak points in the capsule of parotid gland Location Purulent process spread 1 2 3 10.15. Using Fig. 10.12, name the muscles of mastication. What nerves innervate them? Fig. 10.12. Mastication muscles. Frontal aspect mastication muscles № on the fig 2 name 4 6 7 10.16. Name the borders of the deep parotid-masseteric region: Lateral_ _ Medial_ _ Superior_ _ Inferior_ _ innervation 10.17. Using Fig. 10.12 and 10.13, list the fascial cellular spaces of the face and fill in the table. cellular spaces of the head region name: located between: contains structures: 1. Masticatory-mandibular space 2. Pterygo-mandibular space (spatirum temporopterygoideum) 3. Inter-pterygoid space (spatium interpterygoideum) 4. Peri-pharyngeal space (spatium peripharyngeum) Fig. 10.13. Fascial cellular spaces of the face associated with spaces: 10.18. List the sections and branches of the maxillary artery (Fig. 10.14). Fig. 10.14. Maxillary artery The artery sections are:_ _ _ branches of the maxillary artery № № name 1 7 2 8 3 9 4 10 5 11 6 12 name 13 10.19. Using Fig. 10.15, list the branches of the mandibular nerve. What is the mandibular or inferior alveolar nerve block?_ _ What medical specialty can perform this procedure and for what purpose?_ _ Fig. 10.15. Branches of the mandibular nerve 10.20. Fig. 10.16 shows surgical incisions used for draining purulent facial processes. Explain the directions used for these incisions__ _ _ What is the technique for opening and draining retropharyngeal abscess?_ _ _ Fig. 10.16. Facial incisions 11. TOPOGRAPHIC ANATOMY OF THE NECK Topics of the lesson: Surface landmarks, borders and general description of the neck. Projection of the neurovascular bundles of the neck and the cervical plexus. Triangles of the neck. Fasciae and spaces of the neck. Blood supply, venous drainage, innervation, and lymphatic drainage of neck organs. Reflexogenic areas of the neck. 11.1. Draw the borders of the neck regions in Fig. 11.1, name them: Superior_ _ _ _ _ _ Inferior_ _ _ _ _ _ Fig. 11.1. The neck 11.2. Name the surface landmarks depicted in Fig. 11.1. 11.3. Draw the projective line of the carotid artery in Fig. 11.2, name the content of the neurovascular bundle: Arteries:_ _ Vein:_ _ Nerve:_ _ Fig. 11.2. The projection of the neurovascular bundle of the neck. Triangles of the neck 11.4. Name the regions and 6 triangles of the neck in English and Latin, highlight them in Fig. 11.2. English Latin The anterior region: 1. 2. 3. 4. English Latin The lateral region: 5. 6. 7. 11.5. Highlight the 5 fasciae of the neck in Fig. 11.3 and complete the table. Fig. 11.3. Fasciae of the neck (according to Shevkunenko) facia according according to rna structure covered by fascia to shevkunenko?s classification 1 m. 2 m. m. m. 3 m. m. m. m. 4А a., v., n. 4B 5 m. m. m. 11.6. Complete the table on cellular spaces of the neck. Names in english: Names in latin: Situated within triangle(s): Formed by fascia/ Contain: fasciae: 1 2 3 4 5 6 7 8 9 10 11.7. Put down the names of all the fasciae of the neck triangles depicted in Fig. 11.4. Fig. 11.4. Triangles of the neck 11.8. Using Fig. 11.5, name the external carotid artery brunches. № Artery: 1 2 3 4 5 6 7 8 9 10 11 12 Fig. 11.5. Brunches of the external carotid artery 11.9. In the Fig. 11.6, put down the names of the cervical lymph node. Fig. 11.6. Cervical lymph nodes 11.10. Draw and write down the borders of the Piragoffs triangle. The triangle is used in surgery as an internal landmark at approaching the_ _ _ _ This structure may also be approached by_ _triangle. Fig. 11.7. The Piragoff's triangle 11.11. Complete the table on topography of the sternocleidomastoid region of the neck. Formed by: THE PRESCALENE SPACE THE INTERSCALENE SPACE THE SCALENOVERTEBRAL TRIANGLE Superiorly: _ Superiorly: Medially: Posteriorly: _ Posteriorly: Laterally: Inferiorly: Contents: - arteries: - veins: - nerves: - other structures: 11.12. Using notes from the lectures, complete the table on the reflexogenic areas of the neck. REFLEXOGENIC AREAS TOPOGRAPHY 11.13. Explain the situation in this clinical case. Esophagectomy was performed on a patient with advanced cancer of the lower third of esophagus. Temporary hoarseness was observed after the surgery, but the voice returned to normal in a while. Explain what the symptoms can be connected with. Give topographic and anatomic ground__ _ _ _ _ _ _ 11.14. Complete the table. TOPOGRAPHY OF NECK ORGANS ORGAN SKELETOTOPY SYNTOPY Larynx Superiorly -___________bone BLOOD SUPPLY a a. INNERVATION a. plex. n. n. Anteriorly -____________mm. Posteriorly – Pharynx/cervical region TOPOGRAPHY OF NECK ORGANS Laterally – Anteriorly - Posteriorly Laterally - ORGAN SKELETOTOPY SYNTOPY Trachea Anteriorly – BLOOD SUPPLY INNERVATION a. n. Posteriorly - Laterally Esophagus Anteriorly - Posteriorly Laterally - a. n. Thyroid gland Superiorly - Anteriorly Posteriorly - Laterally - a a. n. a. n. Parathyroid glands Inner landmark - Anteriorly - Posteriorly - 11.15. What nerve damage is shown in Fig. 1.8?_ Fig. 11.8. Tongue innervation disorder _ Which nerve innervates the muscles of the tongue?_ _ Fig. 11.9. Spasmodic torticollis’ 11.16. Fig. 11.9 illustrates the cranial nerves disorder, called 'torticollis'. Identify what nerve is the symptom connected with:_ _ _ Which muscles innervate the nerve?_ _ _ _ 11.17. Using Fig. 11.10, write down which structures are situated within the prescalene and interscalene space. Complete the table. Fig. 11.10. Topography of the interscalene and prescalene space THE INTERSCALENE SPACE THE PRESCALENE SPACE borders: 1 Posteriorly - 2 Posteriorly - 2 Anteriorly - ? Anteriorly - contents: 3 6 4 7 ? 8 10 11.18. Draw the borders of the scalenovertebral space of the neck. Which structures are situated within it? Complete the table. Use Figs. 11.11 and 11.12. Fig. 11.11. Topography of the scalenovertebral space Fig. 11.12. Topography of the scalenovertebral space TOPOGRAPHY OF THE SCALENOVERTEBRAL SPACE А. Borders: THE NAME IN ENGLISH THE NAME IN LATING Lateral - - Medial - - Base - - B. Anatomic structures: Arteries: Veins: Nerves: Duct: 11.19. Using Fig. 11.13, point out from which dural venous sinus does the blood flow to the neck? 2 -_ Which neck vein does it flow into? 8 -_ What main neck veins are depicted in Fig. 11.13? 3 -_ 4 -_ 5 -_ 8 -_ 9 -_ Fig. 11.13. Head and neck veins 11.20. Using Fig. 11.14, fill in the table. Fig. 11.14. Vertebral vein arteries veins nerves A1 V1 N1 A2 V2 N2 A3 V3 N3 N4 12. OPERATIVE SURGERY OF THE NECK Topics of the lesson: Operative access to neck vessels and organs. Openings at neck phlegmons. The vagosympothetic block according to Vishnevsky. The resection on thyroid gland. Larynx and trachea operations. 12.1. Give the definition. Tracheostomy is_ _ _ 12.2. Write down the types of tracheostomy: 1. __ 2. __ 3. __ 12.3. Point out, in what direction the incision for performing tracheostomy is made: _ _ Write down the cellular spaces surrounding the trachea when performing tracheostomy (beside the subcutaneous tissue): 1. __ 2. __ 12.5. Fill in the table: OPERATION: TRACHEOTOMY (TRACHEOSTOMY) 1. Surgical indications: 2. The levels of tracheal ring incision: a) superior tracheostomy: is performed_____________________the isthmus _ b) middle tracheostomy: is performed _ ___________________the isthmus _ c) inferior tracheostomy: is performed ____________________the isthmus _ 3. The position of a patient during the operation: 4. Types of pain relief: 5. The direction of tracheal ring incision: a) b) OPERATION: TRACHEOTOMY (TRACHEOSTOMY) Inferior tracheotomy 6. Operative access: a) to make an incision on_ by 2 inches starting from_using scalpel b) to make an incision of the_ fascia _ _________________________space is opened c) to make an incision of the_ fascia To draw the_ ________________________musclus bylaterally; _ __________________________space is opened d) to pick off the trachea wall in the cellular tissue to manipulate carefully - risk of injuring _______________________________________ ___________________________________, and arteries e) to pick off the isthmus_ f) to draw the isthmus_ using blunt retractor; 7. Tracheostomy: a) take and pull up_ using one-tooth clamps; b) to make an incision_ to put an up to 1 cm stop on the scalpel to prevent _ and_ ________________________________injuring; c) to pull apart the edges using_ d) to enter into the tracheal cavity using_ e) in case of tracheostomy to suture using_ f) to fix the tracheostomy tube_ using_ 8. Breathing is controlled: 9. Gauze stripes are put over suture lines 12.6. What surgery is depicted in Fig. 12.1?_ _ Fig. 12.1. Surgery at larynx Which cartilages are marked in Fig. 12.1? 1 -_ 2 -_ How is this surgery different from tracheostomy?_ _ _ 12.7. Draw the incision line for accessing the cervical esophagus and the retrovisceral space. Fig. 12.2. The position of the head 12.8. What medical device is illustrated in Fig. 12.3? What surgery is it intended for?_ _ _ _ Fig. 12.3. A medical device 12.9. What intraoperarive complications are possible when performing tracheostomy? 1. Hemorrhage from:_ 2. Nerve damage:_ 3__ 4__ 5__ 12.10. What is thyroid resection?_ _ _ In what pathologies is it performed?,_ _ 12.11. Access to what organ of submandibular triangle is illustrated in Fig. 12.4? Fig. 12.4. Access to the submandibular triangle of the neck Which vessels were found and ligated? 1 -_; 2 -_ Is it possible to keep them in the process of accessing? How? _ What nerve might be injured when performing this kind of operative access? 4 -_ What rule is to be followed to prevent it? _ _ _ 12.12. What structures are depicted in Fig. 12.5? Fig. 12.5. Surface landmarks of the neck 1 - v. __ _ 2 - m. __ _ During what surgery is this point of surface landmarks' overlap used? _ _ _ _ _ _ _ _ 12.13. Fill in the table: THE VAGOSYMPATHETIC BLOCKAGE ACCORDING TO VISHNEVSKY 1. Indications: - 2. Patient's position: 3. Needle injection point: 4. The direction of the needle: 5. Blockage technique: 6. The successful block is characterized by the presence of the BernerdHorner?s syndrome: Bernerd-Horner?s syndrome: 1234- 12.14. Fill in the table on the directions of spreading pus. CELLULAR SPACES SPREADING UPWARDS: SPREADING DOWNWARDS: Carotid neurovascular bundle Previsceral Retrovisceral Lateral Deep lateral 12.15. Draw the incision lines of the neck phlegmons in Fig. 12.6. Fill in the table. Fig. 12.6. Incision for at neck phlegmons PHLEGMON OF THE SPACE: 1 • suprasternal space 2 • capsules of the sternocleidomastoid muscle 3 • capsules of the carotid neurovascular bundle 4 • submandibular space 5 • previsceral space 6 • retrovisceral space THE INCISION IS MADE ALONG THE SURFACE LANDMARKS:





